Rheumatoid arthritis vs. osteoarthritis, differences in symptoms, causes, and treatment
 Rheumatoid arthritis and osteoarthritis are just two of the many different types of arthritis. Although there are many commonalities between these conditions – joint pain being a large one – there are important differences between the two that can aid in determining a proper treatment.
Rheumatoid arthritis and osteoarthritis are just two of the many different types of arthritis. Although there are many commonalities between these conditions – joint pain being a large one – there are important differences between the two that can aid in determining a proper treatment.
Here are some key points you need to understand. Rheumatoid arthritis is an autoimmune disease that can affect the entire body, whereas osteoarthritis is a degenerative disease that affects the cartilage between the joints. The goal of treatment for either one is to reduce swelling, pain, and stiffness, and to slow down the progression of joint damage.
Arthritis is a condition that refers to the inflammation affecting the joints, and there are numerous different types of arthritis. The main difference between rheumatoid arthritis and osteoarthritis is that one is an autoimmune disease and the other is a degenerative disease.
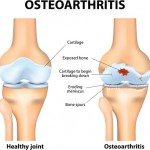
In an autoimmune disorder, the immune system acts wrongly and begins to attack itself – in the case of rheumatoid arthritis, it’s the joints that are under attack. The main characteristic of osteoarthritis, a degenerative disease, is the breakdown of cartilage, which is the cushion found between joints. When the cartilage breaks down, there is no longer any lubrication between bones, which start rubbing together as a result. Both types of arthritis lead to inflammation.
Difference between rheumatoid arthritis and osteoarthritis: Table
Here is a table outlining the main differences between rheumatoid arthritis and osteoarthritis for your reference.
Rheumatoid arthritis Osteoarthritis Type of disease Autoimmune disease – immune system attacks the synovium Degenerative disease – wear and tear of cartilage Symptoms Joint pain, swelling, stiffness, decreased range of motion, fever, fatigue, loss of energy Joint stiffness, pain, decreased range of motion Location of symptoms Occurs in joint pairs – hands, ankles, etc. Common in weight-bearing joints, like hips, knees, and neck Time of day Worsens in the morning and at night after a long day of activity Worsens after a day of activity Age of onset Between 30 and 50 years of age Middle-aged to older adults Prevalence Estimated 1.3 million Americans live with rheumatoid arthritis Estimated 27 million Americans live with osteoarthritisRheumatoid arthritis vs. osteoarthritis: U.S. prevalence
An estimated 1.3 million Americans live with rheumatoid arthritis, and women have higher rates of rheumatoid arthritis than men. Osteoarthritis prevalence in the U.S. amounts to an estimated 27 million people, with majority of patients experiencing osteoarthritis in their knees, followed by hips, then hands.
Comparison between rheumatoid arthritis and osteoarthritis: Incidence, mortality, and costs
Rheumatoid arthritis (RA) Osteoarthritis (OA) Incidence 41 per 100,000 Hand OA: 100 per 100,000 person-yearsHip OA: 88 per 100,000 person-years
Knee OA: 240 per 100,000 person-years Mortality RA accounts for 22 percent of deaths due to arthritis and other rheumatic conditions
40 percent of RA deaths are related to cardiovascular causes
0.2 to 0.3 deaths per 100,000 (less than 500 deaths)
Underestimated because the cases when OA treatment causes death are not accounted for, e.g., gastrointestinal bleeding due to medications Costs $22.3 billion [2005 US Medical Expenditure Panel Survey (MEPS)]
Median lifetime costs of RA: $61,000 to $122,000
Hip and joint replacement: $28.5 billion
Average cost per patient: $2,600
Rheumatoid arthritis vs. osteoarthritis: Signs and symptoms
Signs and symptoms of rheumatoid arthritis are often worse in the morning lasting for around 30 minutes, whereas in osteoarthritis symptoms of stiffness worsen throughout the day. In rheumatoid arthritis, swelling occurs symmetrically (both hands, both ankles, etc.), but swelling is not symmetrical in osteoarthritis.
Common symptoms in rheumatoid arthritis include joint pain, swelling, stiffness, tenderness, prolonged morning stiffness, and reduced range of motion. Osteoarthritis symptoms include joint stiffness, pain, and enlarged joints. The symptoms are not symmetrical.
Rheumatoid arthritis symptoms often occur in smaller joints, such as the hands, whereas osteoarthritis symptoms occur in larger joints, like the hip.
In rheumatoid arthritis, symptoms can also occur in other parts of the body aside from the joints – like skin, eyes, lungs, heart, kidneys, salivary glands, nerve tissue, bone marrow, and blood vessels. In osteoarthritis, only the cartilage between the joints is affected.
As you can see, there are many similarities in signs and symptoms between rheumatoid arthritis and osteoarthritis, but there are key differences that set the two apart.
Causes of osteoarthritis and rheumatoid arthritis
 Rheumatoid arthritis is a type of an autoimmune disease, but it is still unclear as to why or how autoimmune diseases occur. What is known is that the immune system mistakes parts of the body for a virus and begins to attack it. In the case of rheumatoid arthritis, the immune system attacks the synovium.
Rheumatoid arthritis is a type of an autoimmune disease, but it is still unclear as to why or how autoimmune diseases occur. What is known is that the immune system mistakes parts of the body for a virus and begins to attack it. In the case of rheumatoid arthritis, the immune system attacks the synovium.
Osteoarthritis is a wear-and-tear degenerative disease that could be caused by overuse, injury, obesity, hereditary, or through aging. Over time, the cartilage between the joints wears thinner, causing the bones to rub together.
Comparing rheumatoid arthritis and osteoarthritis: Risk factors and complications
Rheumatoid arthritis Osteoarthritis Risk factors- Being a female
- Being over the age of 40
- Family history of RA
- Smoking
- Environmental exposures such as asbestos or silica
- Obesity
- Aging
- Being a female
- Obesity
- Experiencing joint injuries
- Certain occupations that involve repetitive motions
- Genetics
- Bone deformities
Differences between rheumatoid arthritis and osteoarthritis: Diagnosis
Proper diagnosis of rheumatoid arthritis involves a look at the patient’s medical history, their symptoms, a physical examination, blood tests to look for antibodies associated with rheumatoid arthritis, and imaging tests to determine any joint damage.
Diagnosis of osteoarthritis involves reviewing the patient’s symptoms and medical history, physical examination, examining fluid drawn from the joints, X-ray and MRI to look at the cartilage between the joints.
Rheumatoid arthritis vs. osteoarthritis: Treatment
 Treatment for both rheumatoid arthritis and osteoarthritis should begin early in order to prevent future complications. The objectives of rheumatoid arthritis treatment include reducing inflammation, relieving symptoms, preventing joint and organ damage, improving physical function and well-being, and reducing long-term complications.
Treatment for both rheumatoid arthritis and osteoarthritis should begin early in order to prevent future complications. The objectives of rheumatoid arthritis treatment include reducing inflammation, relieving symptoms, preventing joint and organ damage, improving physical function and well-being, and reducing long-term complications.
Rheumatoid arthritis can be treated with medications to ease symptoms like pain and stiffness. This may involve anti-inflammatory and pain medications. Other medications can be prescribed to slow down the progression of rheumatoid arthritis, including corticosteroids, biologics, and JAK inhibitors. Surgery may be required if damage is severe, and the joint must be replaced in order to improve function.
The objectives of osteoarthritis treatment include managing the symptoms, improving joint mobility and flexibility, maintaining a healthy weight, and getting adequate exercise. Physical activity has been shown to be quite beneficial to osteoarthritis patients, as it strengthens and builds muscles thus easing the burden on the joints. Weight management is also important because excess weight adds unnecessary stress to already painful joints.
Other treatment methods for osteoarthritis include physical and occupational therapy to help patients find less painful methods to complete regular tasks, medications like anti-inflammatories and corticosteroids, use of assistive devices like a cane, and surgery if the joint is severely damaged and needs to be replaced.
Your doctor will help you decide on what type of treatment will offer you the greatest success in living with either rheumatoid arthritis or osteoarthritis.
Osteoarthritis onset revealed by interstitial fluid flow in cartilage
Osteoarthritis onset may be detected through changes in the interstitial fluid flow in cartilage, leading to inflammation. Osteoarthritis is a debilitating disease with no cure that can affect anyone at any age, but is common among older age groups. The osteoarthritis diagnosis generally occurs after irreversible symptoms such as joint pain or stiffness kick in. A common treatment for osteoarthritis is joint replacement surgery. Continue reading…
-
The secrets to Lose Pounds a Month
How much do you know about weight loss? This is the most legitimate qu
-
Type 2 diabetes risk higher in women with polycystic ovary syndrome (PCOS) related inflammation
Type 2 diabetes risk is higher in women with polycystic ovary
-
The Healthy Way To Lose Weight
Successful weight loss is not about a qu
-
Is Fast Fat Loss A Myth?
The rise in the number of fast foods joi
-
How To Shed Belly Fat – Quick Tips For A Flat Tummy
How to Lose tummy fat has got to be the top request I get each week fr
-
Figuring out Weight Loss tax Breaks in a World with Donut Sandwiches
If you remember The Simpsons, perhaps you’ll remember an episode
- DON'T MISS
- The 5 Best Weight Loss Products Ever Created
- Do You Have Fat Genes?
- Diet An Ugly 4Letter Word
- A Straightforward, Straightforward, and Fun way to Lose 1 lb/week
- How Can The Best Paleo Diet Book Improve Healthy Eating Habit.
- Exercise less and lose more weight
- The Right Way To Obtain Those 6 Pack That You’ve Often Dreamed Of
- Use the Pyramid to Get Healthy
- Home test to check if you have diabetes
- Do Not Use Slimming Product With Undeclared Drug Ingredients




